'3° Clinical case: Meningioma'
'3° Clinical case: Meningioma'
Abstract
As anticipated in the introductory chapter 'Occlusion and posture', the greatest danger in medical science is to underestimate the vast range of neuromotor responses that are modulated by as many indeterministic biophysical effects and to build clinical axioms on them. This induces the clinician into a deterministic mindset where the axioms are a certainty but, as will be seen during the implementation of Masticationpedia, this language logic model should leave room for a quantum-like language logic where one does not try to limit the uncertainty error with Bayesan statistical models but accept the limit of the probabilistic uncertainty. Following the first approach (classical model), a subject who reports chewing disorders related to a postural disorder is 99.9% (t-student, P-value, etc.) affected by malocclusion while following a quantum-like approach one wonders what is the 'state' of this subject's system beyond the clinical conclusion that it is and will always remain a probabilistic event. As we will see, this innovative quantum-like approach would speed up the diagnostic finalization.
Introduction
As now implicit, this clinical case too, which from now on we will call with a fancy name Balancer' due to its related symptoms of postural and gait disturbance after being prosthetically rehabilitated, will follow the presentation model of the previous clinical cases. The introduction will present topics relating to the diagnostic model in question on which we will make the first conceptual reflections highlighted by our dear and thoughtful Linus. A recent article by Minervini et al.[1] asserts the following: TMD has ligament and muscle connections with the cervical area, therefore these connections have led to the hypothesis that posture problems may influence the development of TMD, [2][3][4][5][6] therefore masticatory cycles should be balanced as unilateral chewing could alter the postural balance of the body. Stabilization splints can bring about neuromuscular balance, removing posterior interference and providing a stable occlusal relationship and an optimization of the centric relationship. The relationship between craniometric posture and TMD has been studied, however, despite the huge number of studies, clinicians and academics still remain unconvinced.[7]
'Centric Relationship and Posture
The conclusion is mandatory: 'however, despite the huge number of studies, clinical and academic remain unconvincing.' This always turns out to be a diplomatic way to avoid trouble but if we carefully read the salient points of this extract it seems that everything derives from a sort of balance due to occlusal stability and an exact Mandibular Centric Relationship. But the question that arises is:
«What Centric Relationship are we talking about!!!»
(perhaps the forced terminal or the guided one but no!! we do the myocentric which is more suitable perhaps using TENS.)Without going into specific topics referred to the reference chapters, we want to highlight the inconsistencies encountered in such important statements of correlation between Centric Relationship and Posture. We report a clinical case already presented in the chapter 'Conclusions on the status quo in the logic of medical language regarding the masticatory system' because it is very relevant to the topic 'Masticatory correlation' which highlights the discrepancy between a manual Centric Relation obtained intraoperatively to fix the mandibular and condylar bone structures in orthognathic surgery and the spatial position called Neuro Evoked Centric Relationship obtained through Transcranial Electric stimulation of the trigeminal roots. Figure 1a shows the spatial position of the jaws after orthognathic surgery in which the positions are established through a manual method of 'Centric Relationship'. The surgeon has no other means than the manual mandibular positioning procedure. Despite bilateral edentulism, which he would face after a few months, the patient was considered to be in excellent occlusal stability. The previous chapters demonstrated that after performing the trigeminal reflexes, the patient's masticatory system was far from intact. In figure 1b an enlarged detail of the incisal area to visualize the mandibular incisal line moved towards the left side of the patient while in figure 1c we see a spatial symmetrization of the mandible (moving towards the right side of the patient) using a "Neuro Evoked Centric Registration" through transcranial electrical stimulation of the trigeminal roots (bRoot-MEPs)
In conclusion, at this point the problem is no longer the correlation between posture and occlusal stability but the correlation between the Centric Relation and occlusal stability because this relationship is the primus movens of the whole pathophysiological phenomenon and if we are not sure of the assertions we cannot go beyond .
«Be careful, therefore, to use the term 'correlation' between Centric Relation and Posture or Occlusal stability and Posture.»
Another recent study Inchingolo et al.[8] asserts the following: the cranial surface electromyography allows the evaluation of the occlusal state and the quantification of the neuromuscular postural balance, thus understanding the dental occlusion from a functional point of view. It therefore represents a diagnostic revolution because it allows you to see what until now was only perceptible by palpation, and therefore not quantifiable.[9] A meta-analysis on the use of sEMG to evaluate the relationships between masticatory muscles and postural muscles found that the correlation between the masticatory system and the muscle activity of other parts of the body can be detected experimentally using sEMG, but this correlation has little clinic relevance .[10] However, Julià-Sánchez et al. found that dental occlusion affects the biomechanical and viscoelastic properties of masticatory and postural muscles using the MyotonPRO® system.[11] The influence of the occlusal state on stability was also demonstrated in an article by Heit et al. who found a significant increase in balance at rest rather than at maximal intercuspidation.[12] These results are consistent with previous studies that used sEMG to measure both the muscle balance of the masticatory muscles and its influence on the activity of some postural muscles. A substantial reduction in resting postural muscle activity (sternocleidomastoid, erector spinae, and soleus) was found in participants with dental malocclusions after balancing with a bite.[13]
Simmetria: When we speak of neuromotor balance in reference to electromyographic procedures, terms such as synchronicity and symmetry are implicitly evoked. Side-to-side symmetry of EMG motor unit discharges is a complex procedure to record and interpret. Many factors come into play and not only the level of muscle contraction but also the type of electrode and electromyographic device used. If the concept of symmetry is focused referring to interferential EMG pattern then the situation is further complicated by the spatio-temporal summation of the motor units which discharge asynchronously and at variable frequency. This can lead to collisions and cancellations of the recordable potential on the skin. The only way to be able to extrapolate a significant data is the Fourier analysis[14] and the Wavelet model[15] which, with the usual limitations of indeterminacy and measurement uncertainty already discussed in other chapters (Kbrain), tries to decompose the already complex signal due to its nature biochemistry and extrapolate information on biophysics. But the question that arises is:
«Are we sure we are dealing with an 'Asymmetry'?»
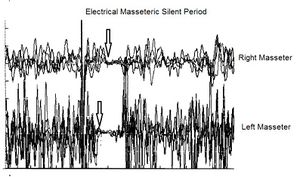
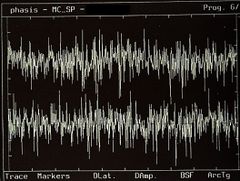
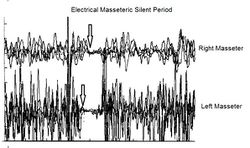
(.... are we talking about a functional or organic asymmetry?)Even with regard to this very delicate point of neuromuscular balance and symmetry, without going into specific topics referred to the reference chapters, we would like to highlight the inconsistencies encountered in statements of the 'symmetry/asymmetry' type between sides of the interferential EMG pattern. Figure 2a shows an interferential EMG trace (right and left masseter, upper and lower trace respectively) in which, obviously, an evident asymmetry can be recognized already at a first visual approach without further mathematical decompositions. In figure 2c, on the other hand, one can also appreciate, in other patient, a good symmetry of the sides.
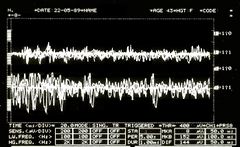
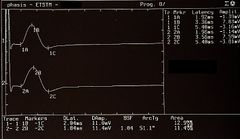
Well, these two asymmetry/symmetry data (figure 2a and 2c) have no clinical significance because they are functional characteristics of the system which, as we anticipated, are unstable and modulated by other internal and external components of the system itself. The clinical and laboratory aspect would change drastically if the interferential EMG pattern content in Figure 2a and 2c were normalized to the content of the Motor Evoked Potential of the trigeminal roots (Figure 2b) - same electrode arrangement). In this way, given the perfect amplitude symmetry of the Root-MEPs, we can irrefutably state that the EMG tracing in figure 2a corresponds to a state of 'Asymmetry' while that of figure 2c to a state of 'Symmetry'. If the bRoot-MEPs were resulted asymmetric we would have had to speak of organic and functional symmetry and not of asymmetry. We should have looked for the causes, perhaps of measurement errors or verifying the extent of the asymmetry of the motor evoked potentials, but the concept is that we cannot give value to a functional peripheral datum without knowing the organic datum.
«Beware of using the term 'Asymmetry' too casually»
(We can say that by throwing a die we have of probability that a number from 1 to 6 comes out but we must be sure that the die has 6 sides and that the numbers are from 1 to 6)
We could go on and on but we prefer to deal with the clinical case of our patient 'Balancer'
3rd Clinical Case
As anticipated we will resume the same diagnostic language presented both for the patient Mary Poppins and for the 'Bruxer' patients so that it becomes an assimilable and practicable model, we will try to superimpose it on the present clinical case called 'Balancer'.
The subject, a 60-year-old man undergoing prosthetic rehabilitation about 10 years earlier, had begun to report masticatory difficulties and specifically a sort of decrease in muscle strength on the right side and slowing down of the masticatory cycle. After an unquantified period of time, the patient also felt a difficulty in both static and dynamic balance. Reporting these disturbances to his dentist, he was proposed a makeover of the prosthetic rehabilitation. The clinical situation did not change, on the contrary the postulated disturbances increased leading the dentist to a new prosthetic rehabilitation this time following the postural methods through a synergism between pedanometric examinations and centric recordings. Having reached our observation, we immediately subjected the patient to our diagnostic process which is, as usual, represented in the form of 'Contexts'.
Meaning of contexts
As already mentioned but it should be emphasized, in the dental field we will have the following sentences and statements to which we give a numerical value to facilitate the treatment, or where it indicates 'normal' and anomaly and therefore a positive report:
Negative TMJ MRI Report in Figure 3, Normal, Negative Report
Negative axiographic report for right condylar tracing in Figure 4, Normality, negative report
Negative axiographic report for left condylar tracing in Figure 5, Normality, negative report.
Slightly asymmetric EMG interference pattern in Figure 6, Abnormality, Positivity Report
In the neurological context we will therefore have the following sentences and assertions to which we give a numerical value to facilitate the treatment and that is where it indicates 'normality' and 'abnormality and therefore positivity of the report:
Absence of jaw jerk in Figure 7 Abnormality, positive report. In clinical situations of occlusal disharmony we could find ourselves faced with situations of amplitude asymmetries that even border on an absence of the jaw jerk but in this clinical case the contextual asymmetry of the interferential EMG could mean nothing. We continue in the neurological context to verify the responses of other trigeminal electrophysiological tests.
Latency asymmetry of the electrical Silent Period on the right masseter in Figure 8, Abnormality, positive report
Demarcator of coherence
As we have already described several times in the previous chapters, the '' is a representative clinical specific weight, complex to research and develop because it varies from discipline to discipline and for pathologies, indispensable in order not to collide logical statements and in diagnostic procedures and fundamental to initialize the decryption of machine language code. In essence, it allows you to confirm the coherence of one assertion against another and vice versa, giving greater weight to the seriousness of the reports and to the choice of the appropriate context.
The weight of the demarcation, therefore, gives greater significance to the more serious assertions in the clinical context from which they derive and therefore beyond the greater or lesser positivity of the assertions or which in any case are always verified and respected, these must be validated on the basis of the clinical severity intrinsic considering the average of the assertions and for one where it indicates 'low seriousness' while 'high seriousness'.
Summarizing in our case 'Balancer' we therefore have:
where
average of the value of clinical statements in the dental context and therefore which derives from positive EMG asymmetry data with respect to the total number and therefore
average of the value of clinical statements in the neurological context and therefore as we have two positive reports out of 2 total
signaling low severity of the dental context
signaling high severity of the neurological context
where the coherence demarcator will define the diagnostic path as follows
As can be seen in our clinical case 'Balancer' we have a diagnostic prevalence towards the neurological context which indicates the neurological component as a diagnostic path.
(because we can confuse a trivial Occlusal-Postural asymmetry with a serious neurological damage of a structural type)
Consequently, we can concentrate on the interception of the tests necessary to decrypt the machine language code that the CNS sends to the outside converted into verbal language which apparently would seem to concern a sort of postural disorder of the dental malocclusion type, due to the incongruous rehabilitation prosthetic. If on the one hand there may be an asymmetry of the interferential EMG of the masseters due to a prosthetic occlusal imbalance, on the other hand such an evident asymmetry of the jaw jerk and the silent period cannot be justified.
Quantum-Like Logic in Medical Diagnostics, Neuromotor Response Modulation, Masticatory Disorders Diagnosis, Postural Disorders and Chewing, Bayesian Statistical Models in Healthcare, Probabilistic Uncertainty in Clinical Conclusions, Centric Relationship and Masticatory System, Temporomandibular Disorders (TMD) and Posture, Diagnostic Criteria for Temporomandibular Disorders, Neuromuscular Balance and Occlusal Stability, Mandibular Centric Relationship Optimization, Craniometric Posture and TMD, EMG Analysis in Dental Occlusion, Surface Electromyography in Dental Diagnostics, Biophysics and Biochemistry in Clinical Diagnostics,
- ↑ Giuseppe Minervini, Rocco Franco, Maria Maddalena Marrapodi, Salvatore Crimi, Almir Badnjević, Gabriele Cervino, Alberto Bianchi, and Marco Cicciù. Correlation between Temporomandibular Disorders (TMD) and Posture Evaluated trough the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): A Systematic Review with Meta-Analysis. J Clin Med. 2023 Apr; 12(7): 2652. Published online 2023 Apr 2. doi: 10.3390/jcm12072652.PMCID: PMC10095000.PMID: 37048735
- ↑ An J.-S., Jeon D.-M., Jung W.-S., Yang I.-H., Lim W.H., Ahn S.-J. Influence of temporomandibular joint disc displacement on craniocervical posture and hyoid bone position. Am. J. Orthod. Dentofac. Orthop. 2015;147:72–79. doi: 10.1016/j.ajodo.2014.09.015.
- ↑ Lee W.Y., Okeson J.P., Lindroth J. The relationship between forward head posture and temporomandibular disorders. J. Orofac. Pain. 1995;9
- ↑ Minervini G., Mariani P., Fiorillo L., Cervino G., Cicciù M., Laino L. Prevalence of temporomandibular disorders in people with multiple sclerosis: A systematic review and meta-analysis. CRANIO® 2022:1–9. doi: 10.1080/08869634.2022.2137129.
- ↑ Minervini G.D., Del Mondo D.D., Russo D.D., Cervino G.D., D’Amico C.D., Fiorillo L.D. Stem Cells in Temporomandibular Joint Engineering: State of Art and Future Persectives. J. Craniofacial Surg. 2022;33:2181–2187. doi: 10.1097/SCS.0000000000008771.
- ↑ Crescente G., Minervini G., Spagnuolo C., Moccia S. Cannabis Bioactive Compound-Based Formulations: New Per-spectives for the Management of Orofacial Pain. Molecules. 2022;28:106. doi: 10.3390/molecules28010106.
- ↑ Abe S., Kawano F., Matsuka Y., Masuda T., Okawa T., Tanaka E. Relationship between Oral Parafunctional and Postural Habits and the Symptoms of Temporomandibular Disorders: A Survey-Based Cross-Sectional Cohort Study Using Propensity Score Matching Analysis. J. Clin. Med. 2022;11:6396. doi: 10.3390/jcm11216396.
- ↑ Alessio Danilo Inchingolo, Carmela Pezzolla, Assunta Patano, Sabino Ceci, Anna Maria Ciocia, Grazia Marinelli, Giuseppina Malcangi, Valentina Montenegro, Filippo Cardarelli, Fabio Piras, Irene Ferrara, Biagio Rapone, Ioana Roxana Bordea, Dario Di Stasio, Antonio Scarano, Felice Lorusso, Andrea Palermo, Kenan Ferati, Angelo Michele Inchingolo, Francesco Inchingolo, Daniela Di Venere, Gianna Dipalma . Experimental Analysis of the Use of Cranial Electromyography in Athletes and Clinical Implications. Int J Environ Res Public Health. 2022 Jun 29;19(13):7975. doi: 10.3390/ijerph19137975.
- ↑ Falla D., Dall’Alba P., Rainoldi A., Merletti R., Jull G. Repeatability of Surface EMG Variables in the Sternocleidomastoid and Anterior Scalene Muscles. Eur. J. Appl. Physiol. 2002;87:542–549. doi: 10.1007/s00421-002-0661-x
- ↑ Perinetti G., Türp J.C., Primožič J., Di Lenarda R., Contardo L. Associations between the Masticatory System and Muscle Activity of Other Body Districts. A Meta-Analysis of Surface Electromyography Studies. J. Electromyogr. Kinesiol. 2011;21:877–884. doi: 10.1016/j.jelekin.2011.05.014.
- ↑ Julià-Sánchez S., Álvarez-Herms J., Cirer-Sastre R., Corbi F., Burtscher M. The Influence of Dental Occlusion on Dynamic Balance and Muscular Tone. Front. Physiol. 2020;10:1626. doi: 10.3389/fphys.2019.01626
- ↑ Heit T., Derkson C., Bierkos J., Saqqur M. The Effect of the Physiological Rest Position of the Mandible on Cerebral Blood Flow and Physical Balance: An Observational Study. Cranio. 2015;33:195–205. doi: 10.1179/0886963414Z.00000000063.
- ↑ Bergamini M., Pierleoni F., Gizdulich A., Bergamini C. Dental Occlusion and Body Posture: A Surface EMG Study. Cranio. 2008;26:25–32. doi: 10.1179/crn.2008.041.
- ↑ Ishii T, Narita N, Endo H.Evaluation of jaw and neck muscle activities while chewing using EMG-EMGtransfer function and EMG-EMG coherence function analyses in healthy subjects.. Physiol Behav. 2016 Jun 1;160:35-42. doi: 10.1016/j.physbeh.2016.03.023. Epub 2016 Apr 5.PMID: 27059322
- ↑ Sharma T, Veer K. EMG classification using wavelet functions to determine muscle contraction.. J Med Eng Technol. 2016;40(3):99-105. doi: 10.3109/03091902.2016.1139202. Epub 2016 Mar 4.PMID: 26942656






![{\displaystyle \delta _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/cd35df3912a48e5b0b70d9cd5b2e1bee432c3272)













![{\displaystyle \gamma _{n}=[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/2f85d0ed73fa3e7903f0321e48668467c1277f4e)















![{\displaystyle \tau =[0|1]}](https://wikimedia.org/api/rest_v1/media/math/render/svg/fbdc534cec0dcf1f070a551e40611eb83e8aca25)










